Cervical cancer is the only cancer that is vaccine-preventable and curable, but the United States is lagging in its efforts to meet the World Health Organization’s 2030 targets to effectively eliminate the disease.
A mix of low vaccination uptake — just 61.7% of U.S. teenage girls were up to date on their HPV vaccine doses in 2022, according to a Centers for Disease Control and Prevention survey — combined with health equity issues have hobbled U.S. efforts to end the disease.
The combination can be deadly: Though cervical cancer is now preventable and treatable, roughly 11,500 new cases are reported in the U.S. each year and roughly 4,000 women die of the disease, according to CDC data.
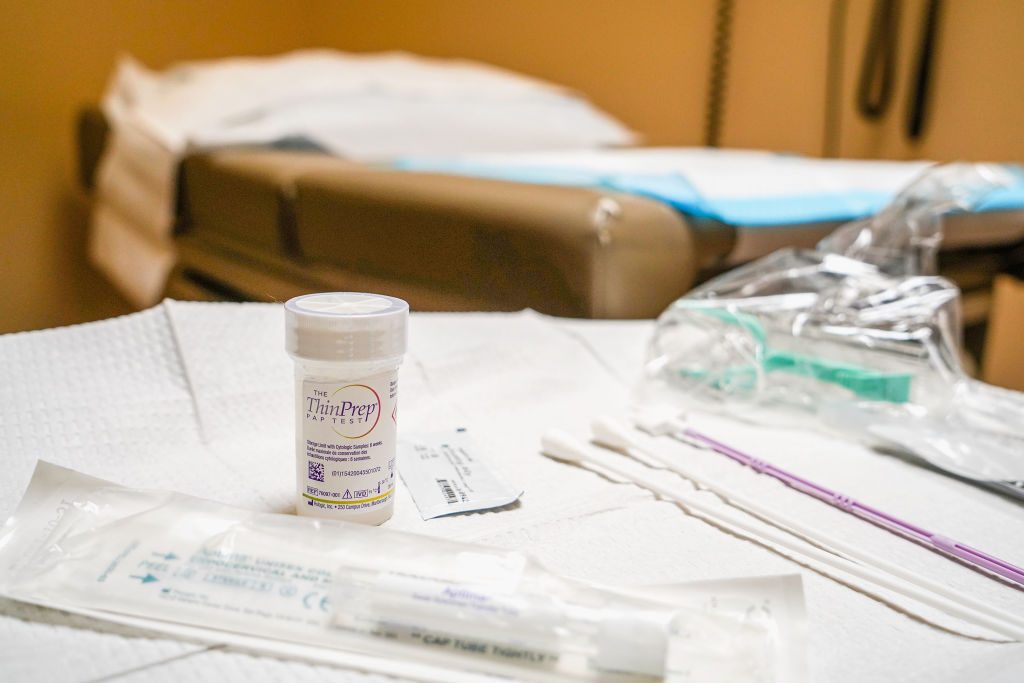
Alarmed by the increase, the Biden administration last week announced a handful of measures aimed at fighting the disease, including a new initiative to lower rates of cervical cancer by allowing for Americans to test for human papillomavirus, or HPV, which causes most cervical cancer, at home.
The new program, called the Self-collection for HPV Testing to Improve Cervical Cancer Prevention, will launch in the second quarter of this year.
The initiative will be a clinical trial network to gather data on the self-collection method of HPV, to prevent cervical cancer.
If the method is determined viable, it could dramatically increase uptake of cervical cancer screening.
Heather White, executive director of TogetHER for Health, an organization that works to eliminate cervical cancer globally, said the Biden administration’s self-sampling initiative could be “a real game changer” for U.S. efforts to stem HPV, because it’ll help get more screenings to women in rural areas and those who may otherwise have issues accessing the health care system.
“That’s a major milestone to be able to turn the regulatory corner,” she said of potential approval of the HPV self-sampling kits. “And I think that’s really where you’ll start to…
Read the full article here