By Stephanie Wolf, KFF Health News
DENVER — Seven years ago, Erica Green learned through a Facebook post that her brother had been shot.
She rushed to check on him at a hospital run by Denver Health, the city’s safety-net system, but she was unable to get information from emergency room workers, who complained that she was creating a disturbance.
“I was distraught and outside, crying, and Jerry came out of the front doors,” she said.
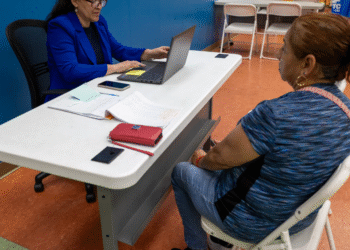
Jerry Morgan is a familiar face from Green’s Denver neighborhood. He had rushed to the hospital after his pager alerted him to the shooting. As a violence prevention professional with the At-Risk Intervention and Mentoring program, or AIM, Morgan supports gun-violence patients and their families at the hospital — as he did the day Green’s brother was shot.
“It made the situation of that traumatic experience so much better. After that, I was, like, I want to do this work,” Green said.
Today, Green works with Morgan as the program manager for AIM, a hospital-linked violence intervention program launched in 2010 as a partnership between Denver Health and the nonprofit Denver Youth Program. It since has expanded to include Children’s Hospital Colorado and the University of Colorado Hospital.
AIM is one of dozens of hospital-linked violence intervention programs around the country. The programs aim to uncover the social and economic factors that contributed to someone ending up in the ER with a bullet wound: inadequate housing, job loss, or feeling unsafe in one’s neighborhood, for example.
Such programs that take a public health approach to stopping gun violence have had success — one in San Francisco reported a fourfold reduction in violent injury recidivism rates over six years. But President Donald Trump’s executive orders calling for the review of the Biden administration’s gun policies and trillions of dollars in federal grants and loans have created uncertainty around the programs’ long-term federal funding….
Read the full article here