Aaron Bolton, MTPR | KFF Health News (TNS)
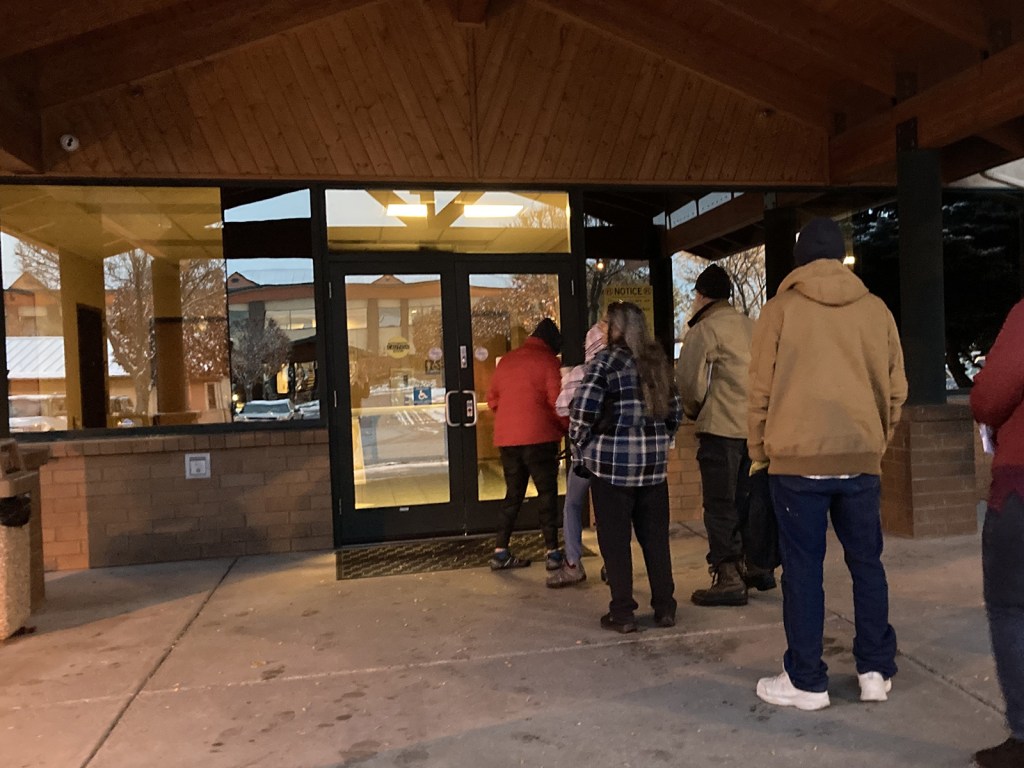
KALISPELL, Mont. — On a cold February morning at the Flathead Warming Center, Tashya Evans waited for help with her Medicaid application as others at the shelter got ready for the day in this northwestern Montana city.
Evans said she lost Medicaid coverage in September because she hadn’t received paperwork after moving from Great Falls, Montana. She has had to forgo the blood pressure medication she can no longer pay for since losing coverage. She has also had to put off needed dental work.
“The teeth broke off. My gums hurt. There’s some times where I’m not feeling good, I don’t want to eat,” she said.
Evans is one of about 130,000 Montanans who have lost Medicaid coverage as the state reevaluates everyone’s eligibility following a pause in disenrollments during the COVID-19 pandemic. About two-thirds of those who were kicked off state Medicaid rolls lost coverage for technical reasons, such as incorrectly filling out paperwork. That’s one of the highest procedural disenrollment rates in the nation, according to a KFF analysis.
Even unsheltered people like Evans are losing their coverage, despite state officials saying they would automatically renew people who should still qualify by using Social Security and disability data.
As other guests filtered out of the shelter that February morning, Evans sat down in a spare office with an application counselor from Greater Valley Health Clinic, which serves much of the homeless population here, and recounted her struggle to reenroll.
She said that she had asked for help at the state public assistance office, but that the staff didn’t have time to answer her questions about which forms she needed to fill out or to walk her through the paperwork. She tried the state’s help line, but couldn’t get through.
“You just get to the point where you’re like, ‘I’m frustrated right now. I just have other things that are more important, and let’s not deal…
Read the full article here