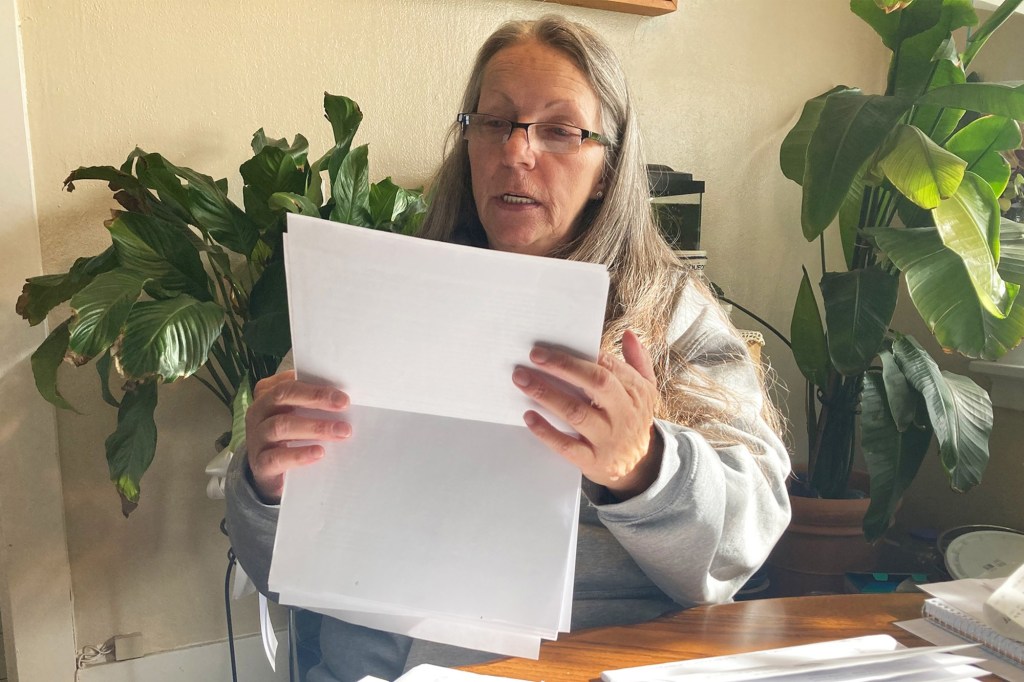
MISSOULA, Mont. — An hour before sunrise, Shelly Brost walked a mile in freezing rain to the public assistance office. She was running out of time to prove she still qualified for food aid after being stymied by a backlogged state call center.
Twice, she’d tried to use Montana’s public assistance help line to complete an interview required to recertify her Supplemental Nutrition Assistance Program, or SNAP, benefits. Each time, the call dropped after more than an hour on hold.
“I was ready to cry,” Brost said as she stood in line with about a dozen other people waiting for the office to open on a recent November morning. “I’ve got a hungry 13-year-old kid.”
Low-income families that need safety-net services, such as food and cash assistance, have become collateral damage in the bureaucratic scramble to determine whether tens of millions of people still qualify for Medicaid after a pandemic-era freeze on disenrollment ended this spring. These are people whose applications and renewal forms have been delayed or lost, or who, like Brost, can’t reach overwhelmed government call center workers.
The impact on services for low-income families is an overlooked consequence of the Medicaid “unwinding,” which has led to coverage being terminated for millions of people since April, with millions more expected to lose coverage in the coming months.
“The Medicaid unwinding has created huge problems for administrative staff,” said Leighton Ku, director of the Center for Health Policy Research at George Washington University’s Milken Institute School of Public Health.
Most states rely on the same workers and computer systems to sort eligibility for Medicaid and SNAP, according to the Center on Budget and Policy Priorities, a left-leaning think tank in Washington, D.C. The difficulty of signing up for other public assistance benefits varies, depending on how each state sets…
Read the full article here